Nursing Care Plan Task
As a nursing student, you will be required to demonstrate core skills on how to write a nursing care plan.
One of the key nursing care plan (NCP) areas you could explore is imbalanced nutrition.
So, how do you approach an imbalanced nutrition less than body requirements NCP?
Imbalanced Nutrition
Per se, imbalanced nutrition is a serious health care problem in nursing practice.
Note that nutritional imbalance results from short or excess supply of certain nutrients.
Accordingly, the imbalance causes undesirable side effects and conditions that usually result into serious disease.
Evidence-based practice for imbalanced nutrition requires the understanding of the micro-and macronutrients needed in the daily diet as well as other foods/nutrients that are not required at all.
For this reason, imbalanced nutrition could assume to forms that include:
1. Imbalanced nutrition: Less than Body Requirements
2. Imbalanced nutrition: More that body requirements
In this case, the imbalance under analysis is “Less than Body Requirements”.
Imbalanced Nutrition: Less than Body Requirements
Before you start writing an imbalanced nutrition less than body requirements NCP, it is important to understand what it entails.
Imbalanced nutrition in the case of Less than Body Requirements can be defined as:
The state where an individual experiences or suffers the risk of experiencing reduced weight due to insufficient intake or metabolism of nutrients necessary for the body’s metabolic needs.
NANDA definition is:
Accordingly, the body requires the right type and amount of nutrients to function appropriately. It has been observed that there are several causes of imbalance in nutrition for less than body requirements.
Per se, just like a nursing care plan for bleeding risk, nursing care plan for urinary retention, nursing care plan for nausea, or nursing care plan for pneumonia, an Imbalanced Nutrition Nursing Care Plan: Less than Body Requirements is quite common in nursing practice and nursing school.
Defining Characteristics
You cannot write an imbalanced nutrition less than body requirements NCP without understanding the defining characteristics first.
When conducting a nutrition nursing diagnosis NANDA for less than body requirements, you need to understand the different defining characteristics.
Usually, defining characteristics include: 1) subjective indicators and 2) objective indicators.
Subjective Indicators
Subjective indicators associated with Imbalanced Nutrition Less Than Body Requirements include:
- Weakness
- Low energy levels
- Difficulty concentrating
- Lack of appetite
- Depression
Objective Indicators
The objective indicators associated with Imbalanced Nutrition Less Than Body Requirements include:
- Weight loss
- Fatigue
- Dry skin
- Thin hair
- Anemia
Associated Conditions
Malnourishment can have far-reaching impacts on a person’s health. People who are not receiving the necessary nutrition are more susceptible to the following conditions:
- Weak bones and muscles
- Anemia
- Fatigue
- Low blood pressure
- Immune system deficiencies
- Slow wound healing
- Susceptibility to infections and diseases
Related Factors
As well, related factors are central to an Imbalanced Nutrition Nursing Care Plan: Less than Body Requirements.
Any evidence-based practice for imbalanced nutrition requires an understanding of the relevant related factors.
Some common related factors relevant to imbalanced nutrition nursing diagnosis NANDA for less than body requirements include:
1. Lack of ability to digest foods.
2. Lack of ability to ingest foods.
3. Lack of ability to metabolize or absorb foods.
4. Lack of ability to access adequate amounts of foods.
5. Lack of proper knowledge.
6. Lack of willingness to eat.
7. High metabolic needs due to therapy or disease process.
Note that your Imbalanced Nutrition Nursing Care Plan: Less than Body Requirements should group related factors in the below major categories.
Situational
These are the different factors that are related to the individual or their environment. They include:
1. Factors related to a decline in eating desire secondary to:
a. Anorexia
b. Allergies
c. Social isolation
d. Stress
e. Depression
2. Factors related to diarrhea.
a. Factors related to lack of ability to access food due to limitations such as financial, physical, or transportation.
b. Factors related to lack of chewing ability due to missing or damaged teeth or ill-fitting dentures.
Treatment Related
These entail an important set of related factors that the Imbalanced Nutrition Nursing Care Plan: Less than Body Requirements should consider.
They entail:
1. Factors related to insufficient absorption that could be a medication side effect associated with:
a. Neomycin
b. Colchicine
c. Antacid
d. Pyrimethamine
e. Para-Aminosalicylic acid
f. Antibiotics such as Rifampicin or Clotrimazole
g. Antihypertensives such as spironolactone or nifedipine
h. Antiepileptics
i. Antiretroviral drugs such as saquinavir or ritonavir
j. Antineoplastic drugs
k. Dexamethasone
l. Colchicine
m. Herbal medicines such as Kava kava
n. Hyperforin
2. Factors related to vitamin and protein requirements required for wound healing and low intake secondary to:
a. Radiotherapy
b. Chemotherapy
c. Wired jaw
d. Surgery
e. Mouth reconstruction through surgery
3. Factors related to mouth discomfort, decline in oral intake, nausea, and vomiting due to:
a. Oral trauma
b. Chemotherapy
c. Tonsillectomy
d. Radiotherapy
Maturational Related
This is another set of factors to consider in your Imbalanced Nutrition Nursing Care Plan: Less than Body Requirements. It particularly focuses on infants or breastfeeding mothers.
Related factors entail:
1. Factors related to insufficient intake due to:
a. Caregiver’s lack of knowledge
b. Insufficient breast milk production
c. Emotional or sensory deficiency
2. Factors related to sucking complications and dysphagia due to:
a. Neurologic impairment
b. Cerebral palsy
c. Cleft lip and palate
3. Factors related to dietary restrictions, malabsorption, and anorexia due to:
a. Cystic fibrosis
b. Celiac disease
c. Lactose intolerance
d. GI malformation
e. Necrotizing enterocolitis
g. Gatroesophageal reflux
4. Factors related to fatigue, inadequate sucking, and dyspnea due to:
a. Developmental challenges
b. Congenital heart disease
c. Prematurity
d. Hyperbilirubinemia
e. Viral syndrome
f. Respiratory distress syndrome
Goals and Outcomes
When writing an imbalanced nutrition less than body requirements, what should be your goals and outcomes?
Evidence-based practice for imbalanced nutrition requires you to develop goals and outcomes for the nursing care plan.
Accordingly, some of the goals and outcomes for Imbalanced Nutrition Nursing Care Plan: Less than Body Requirements include:
1. Patient exhibits comprehension of the importance of nutrition in healing and overall health.
2. Patient exhibits change in behavior and lifestyle in favor of recovery and adoption of suitable weight.
3. Patient and/or caregiver verbally demonstrates the understanding in selection of foods and meals suitable for acquisition of appropriate weight.
4. Patient exhibits consumption of adequate nutrition for metabolic needs as reflected in appropriate weight or tissue regeneration, positive nitrogen balance, muscle-mass measurements, and enhanced energy levels.
5. Patient consumes sufficient amounts of nutrients and calories.
6. Patient exhibits zero malnutrition signs.
7. Patient exhibits weight gain when working towards attainment of set goal as reflected in laboratory values normalization.
8. Patient remains within 10% ideal body weight range.
Nursing Assessment
How do you approach nursing assessment when writing an imbalanced nutrition less than body requirements NCP?
Note that developing an Imbalanced Nutrition Nursing Care Plan: Less than Body Requirements requires you to come up with the right assessment.
A nutrition nursing diagnosis NANDA-aligned should identify all the problems that have the potential to cause the respective imbalanced nutrition.
Assessment should be as illustrated below.
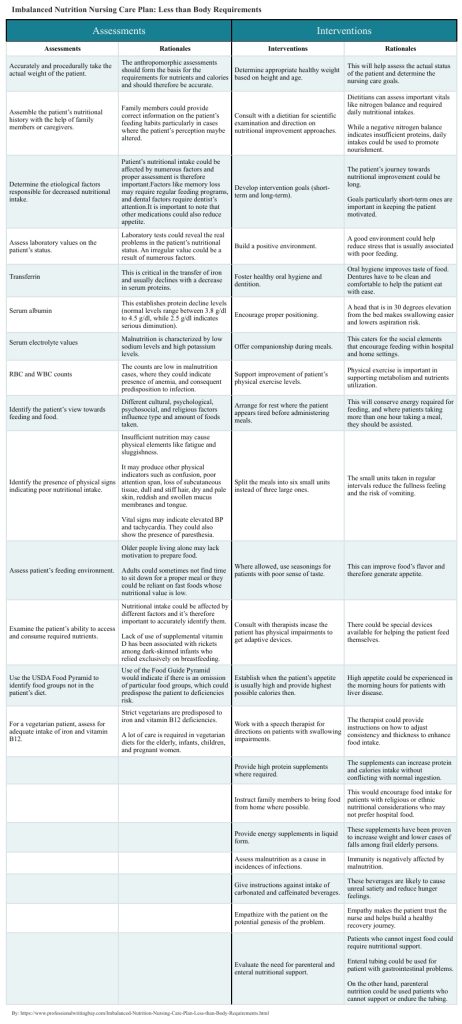
| Assessments | Scientific Rationales |
| Accurately and procedurally take the actual weight of the patient. | The anthropomorphic assessments should form the basis for the requirements for nutrients and calories and should therefore be accurate. |
| Assemble the patient’s nutritional history with the help of family members or caregivers. | Family members could provide correct information on the patient’s feeding habits particularly in cases where the patient’s perception maybe altered. |
| Determine the etiological factors responsible for decreased nutritional intake. | Patient’s nutritional intake could be affected by numerous factors and proper assessment is therefore important.
Factors like memory loss may require regular feeding programs, and dental factors require dentist’s attention. It is important to note that other medications could also reduce appetite. |
| Assess laboratory values on the patient’s status. | Laboratory tests could reveal the real problems in the patient’s nutritional status. An irregular value could be a result of numerous factors. |
| This is critical in the transfer of iron and usually declines with a decrease in serum proteins. |
| This establishes protein decline levels (normal levels range between 3.8 g/dl to 4.5 g/dl, while 2.5 g/dl indicates serious diminution). |
| Malnutrition is characterized by low sodium levels and high potassium levels. |
| The counts are low in malnutrition cases, where they could indicate presence of anemia, and consequent predisposition to infection. |
| Identify the patient’s view towards feeding and food. | Different cultural, psychological, psychosocial, and religious factors influence type and amount of foods taken. |
| Identify the presence of physical signs indicating poor nutritional intake. | Insufficient nutrition may cause physical elements like fatigue and sluggishness.
It may produce other physical indicators such as confusion, poor attention span, loss of subcutaneous tissue, dull and stiff hair, dry and pale skin, reddish and swollen mucus membranes and tongue. Vital signs may indicate elevated BP and tachycardia. They could also show the presence of paresthesia. |
| Assess patient’s feeding environment. | Older people living alone may lack motivation to prepare food.
Adults could sometimes not find time to sit down for a proper meal or they could be reliant on fast foods whose nutritional value is low. |
| Examine the patient’s ability to access and consume required nutrients. | Nutritional intake could be affected by different factors and it’s therefore important to accurately identify them.
Lack of use of supplemental vitamin D has been associated with rickets among dark-skinned infants who relied exclusively on breastfeeding. |
| Use the USDA Food Pyramid to identify food groups not in the patient’s diet. | Use of the Food Guide Pyramid would indicate if there is an omission of particular food groups, which could predispose the patient to deficiencies risk. |
| For a vegetarian patient, assess for adequate intake of iron and vitamin B12. | Strict vegetarians are predisposed to iron and vitamin B12 deficiencies.
A lot of care is required in vegetarian diets for the elderly, infants, children, and pregnant women. |
Nursing Interventions
Nursing interventions are an important part of your imbalanced nutrition less than body requirements NCP.
After the nursing assessment, the Imbalanced Nutrition Nursing Care Plan: Less than Body Requirements should go ahead to provide respective nursing interventions.
These interventions should be as elaborated below.
| Interventions | Scientific Rationales |
| Determine appropriate healthy weight based on height and age. | This will help assess the actual status of the patient and determine the nursing care goals. |
| Consult with a dietitian for scientific examination and direction on nutritional improvement approaches. | Dietitians can assess important vitals like nitrogen balance and required daily nutritional intakes.
While a negative nitrogen balance indicates insufficient proteins, daily intakes could be used to promote nourishment. |
| Develop intervention goals (short-term and long-term). | The patient’s journey towards nutritional improvement could be long.
Goals particularly short-term ones are important in keeping the patient motivated. |
| Build a positive environment. | A good environment could help reduce stress that is usually associated with poor feeding. |
| Foster healthy oral hygiene and dentition. | Oral hygiene improves taste of food. Dentures have to be clean and comfortable to help the patient eat with ease. |
| Encourage proper positioning. | A head that is in 30 degrees elevation from the bed makes swallowing easier and lowers aspiration risk. |
| Offer companionship during meals. | This caters for the social elements that encourage feeding within hospital and home settings. |
| Support improvement of patient’s physical exercise levels. | Physical exercise is important in supporting metabolism and nutrients utilization. |
| Arrange for rest where the patient appears tired before administering meals. | This will conserve energy required for feeding, and where patients taking more than one hour taking a meal, they should be assisted. |
| Split the meals into six small units instead of three large ones. | The small units taken in regular intervals reduce the fullness feeling and the risk of vomiting. |
| Where allowed, use seasonings for patients with poor sense of taste. | This can improve food’s flavor and therefore generate appetite. |
| Consult with therapists incase the patient has physical impairments to get adaptive devices. | There could be special devices available for helping the patient feed themselves. |
| Establish when the patient’s appetite is usually high and provide highest possible calories then. | High appetite could be experienced in the morning hours for patients with liver disease. |
| Work with a speech therapist for directions on patients with swallowing impairments. | The therapist could provide instructions on how to adjust consistency and thickness to enhance food intake. |
| Provide high protein supplements where required. | The supplements can increase protein and calories intake without conflicting with normal ingestion. |
| Instruct family members to bring food from home where possible. | This would encourage food intake for patients with religious or ethnic nutritional considerations who may not prefer hospital food. |
| Provide energy supplements in liquid form. | These supplements have been proven to increase weight and lower cases of falls among frail elderly persons. |
| Assess malnutrition as a cause in incidences of infections. | Immunity is negatively affected by malnutrition. |
| Give instructions against intake of carbonated and caffeinated beverages. | These beverages are likely to cause unreal satiety and reduce hunger feelings. |
| Empathize with the patient on the potential genesis of the problem. | Empathy makes the patient trust the nurse and helps build a healthy recovery journey. |
| Evaluate the need for parenteral and enteral nutritional support. | Patients who cannot ingest food could require nutritional support.
Enteral tubing could be used for patient with gastrointestinal problems. On the other hand, parenteral nutrition could be used patients who cannot support or endure the tubing. |
Imbalanced Nutrition Nursing Care Plan: Less than Body Requirements