Risk for Bleeding
Risk for bleeding is a major concern in nursing practice.
Note that the risk for bleeding is likely to occur when a disease or disease treatment outcomes confuse the standard human body mechanisms charged with the responsibility of maintaining hemostasis.
- Risk for Bleeding
- What is Risk for Bleeding
- Risk Factors
- Goals of a Nursing Care Plan for Bleeding Risk
- Outcomes of a Nursing Care Plan for Bleeding Risk
- NOC Outcomes for a Nursing Care Plan for Bleeding Risk
- Assessment in Nursing Care Plan for Bleeding Risk
- Interventions in Nursing Care Plan for Bleeding Risk
What is Risk for Bleeding
Generally, a risk for bleeding definition could be:
The risk for a decrease in blood volume that may compromise an individual’s health.
Markedly, just like a nursing care plan for pneumonia, a risk for nursing diagnosis, or EBP in nursing, nursing care plan for bleeding risk is a common assignment in nursing schools.
At one point in your studies you will be required to write a nursing essay on a nursing care plan for bleeding risk to help develop your care plan skills as well as assess acquisition and development of requisite knowledge and skills.
In this, you are required to demonstrate your knowledge in areas such as types of bleeding, NANDA nursing diagnosis for bleeding, and NANDA nursing care plans.
This as well demands good skills on how to write a nursing care plan.
Risk Factors
Developing a nursing care plan for bleeding risk requires an understanding of the entailed risk factors. These factors encompass some of the most common types of bleeding.
Per se, key risk factors may include:
1. Postpartum complications like retained placenta or uterine atony
2. Complications related to pregnancy, including abruption, multiple gestation, or placenta preavia
3. Side effects related to treatment like chemotherapy, surgery, medications with effects on clotting and bleeding, and platelet-deficient blood products administration
4. Disseminated intravascular coagulopathy
5. Circumcision
6. Gastrointestinal disorders like varices, polyps, or gastric ulcers
7. Inherent coagulopathies such as hemophilia and thrombocytopenia
8. Impaired liver function diseases or conditions like hepatitis or cirrhosis
9. Aneurysm
10. Trauma or history of falls
Goals of a Nursing Care Plan for Bleeding Risk
All NANDA nursing care plans are guided by specific goals. In this particular case, the goals play an in important role in guiding NANDA nursing diagnosis for bleeding. These goals are as illustrated below.
1. Prevention of bleeding: This entails enabling the affected individual to take bleeding preventive measures as well as recognize bleeding signs that need immediate reporting to the right health care professional.
2. Ensuring absence of bleeding: This is an important goal in risk for bleeding NANDA nursing care plans. It encompasses ensuring there is no bleeding by boosting stable hemoglobin and hematocrit levels, normal blood pressure, and appropriate coagulation profile levels.
Outcomes of a Nursing Care Plan for Bleeding Risk
Based on the above NANDA nursing diagnosis for bleeding goals, a nurse can go ahead and come up with a list of expected outcomes.
In terms of patient behavior, such outcomes include:
1. Receiving screening necessary for creating alerts on existing bleeding risk factors.
2. Receiving the appropriate follow-through intervention.
3. Maintaining heart blood pressure, rhythm, rate, and tissue perfusion within appropriate ranges during episode risks.
4. Receiving appropriate staffing and surveillance from clinicians for rapid response necessary in rescuing the patient before the occurrence of serious bleeding.
5. Identifying and avoiding risk situations that have trauma injury potential.
NOC Outcomes for a Nursing Care Plan for Bleeding Risk
As well, good risk for bleeding NANDA nursing care plans should consider Nursing Outcomes Classification (NOC).
Such outcomes could be categorized as below.
1. Blood coagulation
2. Knowledge- medication
3. Knowledge- disease control
4. Risk control
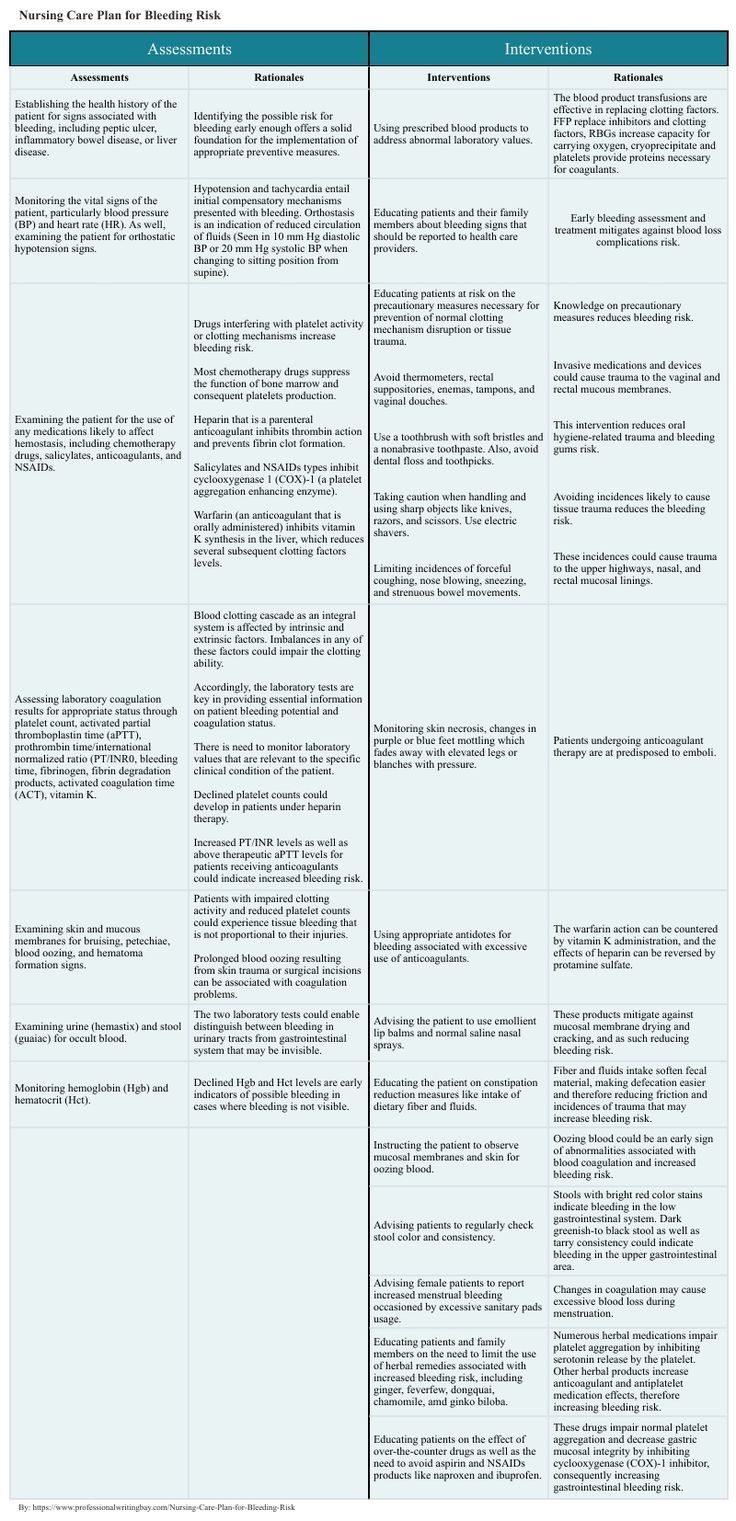
Assessment in Nursing Care Plan for Bleeding Risk
Now that you understand bleeding definition and the respective types of bleeding, it is important that you go ahead and explore the assessment of the bleeding risk.
This assessment is critical in identifying potential problems likely to have caused the bleeding and the event that may arise during the nursing care process.
The assessments together with the corresponding rationales are as illustrated below.
| Assessments | Rationales |
| Establishing the health history of the patient for signs associated with bleeding, including peptic ulcer, inflammatory bowel disease, or liver disease. | Identifying the possible risk for bleeding early enough offers a solid foundation for the implementation of appropriate preventive measures. |
| Monitoring the vital signs of the patient, particularly blood pressure (BP) and heart rate (HR). As well, examining the patient for orthostatic hypotension signs. | Hypotension and tachycardia entail initial compensatory mechanisms presented with bleeding. Orthostasis is an indication of reduced circulation of fluids (Seen in 10 mm Hg diastolic BP or 20 mm Hg systolic BP when changing to sitting position from supine). |
| Examining the patient for the use of any medications likely to affect hemostasis, including chemotherapy drugs, salicylates, anticoagulants, and NSAIDs. | Drugs interfering with platelet activity or clotting mechanisms increase bleeding risk.
Most chemotherapy drugs suppress the function of bone marrow and consequent platelets production. Heparin that is a parenteral anticoagulant inhibits thrombin action and prevents fibrin clot formation. Salicylates and NSAIDs types inhibit cyclooxygenase 1 (COX)-1 (a platelet aggregation enhancing enzyme). Warfarin (an anticoagulant that is orally administered) inhibits vitamin K synthesis in the liver, which reduces several subsequent clotting factors levels. |
| Assessing laboratory coagulation results for appropriate status through platelet count, activated partial thromboplastin time (aPTT), prothrombin time/international normalized ratio (PT/INR0, bleeding time, fibrinogen, fibrin degradation products, activated coagulation time (ACT), vitamin K. | Blood clotting cascade as an integral system is affected by intrinsic and extrinsic factors. Imbalances in any of these factors could impair the clotting ability.
Accordingly, the laboratory tests are key in providing essential information on patient bleeding potential and coagulation status. There is need to monitor laboratory values that are relevant to the specific clinical condition of the patient. Declined platelet counts could develop in patients under heparin therapy. Increased PT/INR levels as well as above therapeutic aPTT levels for patients receiving anticoagulants could indicate increased bleeding risk. |
| Examining skin and mucous membranes for bruising, petechiae, blood oozing, and hematoma formation signs. | Patients with impaired clotting activity and reduced platelet counts could experience tissue bleeding that is not proportional to their injuries.
Prolonged blood oozing resulting from skin trauma or surgical incisions can be associated with coagulation problems. |
| Examining urine (hemastix) and stool (guaiac) for occult blood. | The two laboratory tests could enable distinguish between bleeding in urinary tracts from gastrointestinal system that may be invisible. |
| Monitoring hemoglobin (Hgb) and hematocrit (Hct). | Declined Hgb and Hct levels are early indicators of possible bleeding in cases where bleeding is not visible. |
Interventions in Nursing Care Plan for Bleeding Risk
Proper bleeding risk NANDA nursing care plans have to come up with elaborate interventions. The interventions are supposed to be in line with the assessments made.
That said, such interventions and their rationales maybe as illustrated below.
| Interventions | Rationales |
| Using prescribed blood products to address abnormal laboratory values. | The blood product transfusions are effective in replacing clotting factors. FFP replace inhibitors and clotting factors, RBGs increase capacity for carrying oxygen, cryoprecipitate and platelets provide proteins necessary for coagulants. |
| Educating patients at risk on the precautionary measures necessary for prevention of normal clotting mechanism disruption or tissue trauma.
Avoid thermometers, rectal suppositories, enemas, tampons, and vaginal douches.
Use a toothbrush with soft bristles and a nonabrasive toothpaste. Also, avoid dental floss and toothpicks.
Taking caution when handling and using sharp objects like knives, razors, and scissors. Use electric shavers.
Limiting incidences of forceful coughing, nose blowing, sneezing, and strenuous bowel movements. | Knowledge on precautionary measures reduces bleeding risk.
Invasive medications and devices could cause trauma to the vaginal and rectal mucous membranes.
This intervention reduces oral hygiene-related trauma and bleeding gums risk.
Avoiding incidences likely to cause tissue trauma reduces the bleeding risk.
These incidences could cause trauma to the upper highways, nasal, and rectal mucosal linings. |
| Educating patients and their family members about bleeding signs that should be reported to health care providers. | Early bleeding assessment and treatment mitigates against blood loss complications risk. |
| Monitoring skin necrosis, changes in purple or blue feet mottling which fades away with elevated legs or blanches with pressure. | Patients undergoing anticoagulant therapy are at predisposed to emboli. |
| Using appropriate antidotes for bleeding associated with excessive use of anticoagulants. | The warfarin action can be countered by vitamin K administration, and the effects of heparin can be reversed by protamine sulfate. |
| Advising the patient to use emollient lip balms and normal saline nasal sprays. | These products mitigate against mucosal membrane drying and cracking, and as such reducing bleeding risk. |
| Educating the patient on constipation reduction measures like intake of dietary fiber and fluids. | Fiber and fluids intake soften fecal material, making defecation easier and therefore reducing friction and incidences of trauma that may increase bleeding risk. |
| Instructing the patient to observe mucosal membranes and skin for oozing blood. | Oozing blood could be an early sign of abnormalities associated with blood coagulation and increased bleeding risk. |
| Advising patients to regularly check stool color and consistency. | Stools with bright red color stains indicate bleeding in the low gastrointestinal system. Dark greenish-to black stool as well as tarry consistency could indicate bleeding in the upper gastrointestinal area. |
| Advising female patients to report increased menstrual bleeding occasioned by excessive sanitary pads usage. | Changes in coagulation may cause excessive blood loss during menstruation. |
| Educating patients and family members on the need to limit the use of herbal remedies associated with increased bleeding risk, including ginger, feverfew, dongquai, chamomile, amd ginko biloba. | Numerous herbal medications impair platelet aggregation by inhibiting serotonin release by the platelet. Other herbal products increase anticoagulant and antiplatelet medication effects, therefore increasing bleeding risk. |
| Educating patients on the effect of over-the-counter drugs as well as the need to avoid aspirin and NSAIDs products like naproxen and ibuprofen. | These drugs impair normal platelet aggregation and decrease gastric mucosal integrity by inhibiting cyclooxygenase (COX)-1 inhibitor, consequently increasing gastrointestinal bleeding risk. |
Nursing Care Plan for Bleeding Risk